A widely available and inexpensive antidepressant could soon save lives from a very different kind of disease.
The growth of the most aggressive and deadly brain cancer, glioblastoma, was effectively suppressed in both cases ex vivo human tissue samples and in living mice an FDA-approved serotonin modulator currently used to treat major depression.
It is not a cure, but it can provide some relief and be an effective part of a treatment regimen for glioblastoma patients. Clinical trials on humans are the next step; patients are warned against self-medication at this stage.
“The advantage of vortioxetine is that it is safe and very cost-effective,” says neurologist Michael Weller from the University Hospital Zurich in Switzerland. “Since the drug has already been approved, it does not need to undergo a complicated approval process and could soon complement the standard therapy for this deadly brain tumor.”
Glioblastoma is rare, but when it strikes, it’s hard to beat. The tumor usually appears on the brain or brain stem and grows quickly and aggressively. There is currently no cure, which means it is usually fatal 95 percent of patients within five years. Treatment usually includes radiotherapy and chemotherapy sometimes surgery try to remove as much of the tumor as is safe.
A non-invasive treatment that can complement existing interventions to improve outcomes is something doctors would like to have, but since few cancer drugs can cross the blood-brain barrier, options are limited.
A team of researchers led by molecular biologist Sohyon Lee from ETH Zurich uses cultured human tissue grown from samples donated by glioblastoma patients undergoing treatment surgery, to see whether existing drugs could be effective in suppressing the growth of cancer cells. They focused mainly on antidepressants, antipsychotics and medications used to treat Parkinson’s disease.
In total, they tested 132 drugs on tissue from 27 glioblastoma patients, cataloging more than 2,500 drug reactions. And they found, surprisingly, that some antidepressants were effective at suppressing the development of cancer cells, including a serotonin cell.a modulator called vortioxetine.
One of the actions of vortioxetine is: activate signaling cascadesa series of responses in a cell that are initiated by a stimulus. These cascades suppress cell division, which is how cancer grows and spreads.
Computer simulations showed that the simultaneous cascade of neural cells and cancer cells was necessary to inhibit the cancer. Therefore, only some antidepressants were effective; they don’t all work the same way.
The next step was to test the drugs in a living respiratory system: mice with glioblastoma. Mice were transplanted with glioblastoma tumors and then assigned to a group. The control group was left untreated, while a second group of mice were treated with the SSRI antidepressant citalopram. Finally, a third group was treated with vortioxetine.
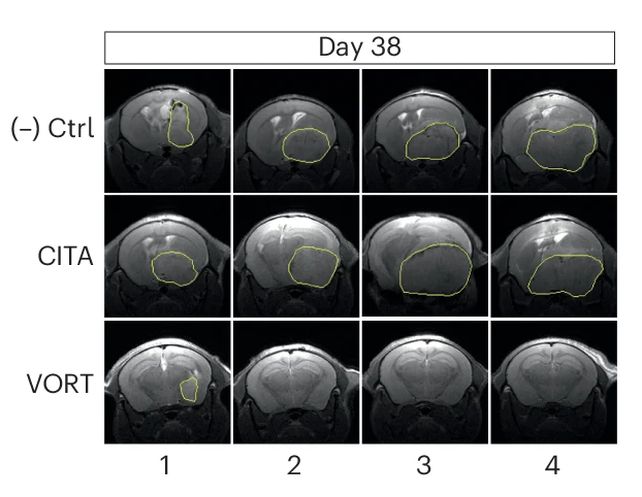
Comparisons made 38 days after tumor implantation showed that the vortioxetine-treated group had significantly less tumor growth and invasiveness than the control group and the citalopram group, which showed similar results.
In a follow-up experiment, another sample of glioblastoma mice was treated with standard chemotherapy drugs. Another group received vortioxetine, while a third group did not.has not received any other treatment.
Likewise, the vortioxetine group had survival rates 20-30 percent higher than those of the chemo-only group, not only in the short term, but also in the long term.
With such promising preclinical results, additional studies in living human patients could reveal whether we may already have a glioblastoma therapy ready for accelerated development.
“We don’t yet know whether the drug works in people and what dose is needed to fight the tumor. That is why clinical trials are needed.” Weller warns. “Self-medication would be an incalculable risk.”
Nevertheless, the drug shows more promise for treating this devastating cancer than we’ve seen in a while, giving some hope to the estimated 250,000 people diagnosed with glioblastoma each year.
“We started with this terrible tumor and found existing drugs that fight it,” says molecular biologist Berend Snijder from ETH Zurich. “We’re showing how and why they work, and soon we’ll be able to test them on patients.”
The research was published in Naturopathy.



